Covid-19
Omicron and the BA.2 Subvariant: What We Know
Over the past several months, COVID-19 has progressed rapidly. Omicron emerged last fall just after Delta had gone past its peak and people were preparing for Thanksgiving. There were fewer cases of illness and death with the new variant than Delta. The variant was also very contagious-more contagious than the one before.
Then, in the early months of 2022, experts turned their attention to Omicron BA.2, a genetically distinct variant of Omicron (or BA.1), which quickly rose to prominence in the United States. Toward the end of April, they began watching subvariants that split off from BA.2. Two of these are not multiplying at this time in the United States. There are other subvariants as well, BA.2.12.1, which accounts for 20% of new cases.
The newest variants are still being studied to determine if they are more contagious or dangerous. There are no reports of serious illness or death caused by BA.2.12.1 so far.
It can become difficult to track these variants – even overwhelming – but Yale Medicine keeps track of them, and the CDC provides weekly updates.
Among the experts in pediatric infectious diseases, Dr. Thomas Murray, PhD, of Yale Medicine, and Dr. Nathan Grubaugh, PhD, of the Yale School of Public Health, commented.
Related News: UK’s COVID Alert Level Reduced As Omicron Sub-types Surface
Omicron: An increase in COVID-19 cases and possibly different symptoms
A little background first. Botswana, South Africa, and the Netherlands were the first countries to report Omicron cases in November. Last year, a case was reported in California on Dec. 1. As of late December, it had become the dominant strain in the United States. In November 2021, scientists found BA.2, and the first case was reported in the U.S. in January. Both organizations have classified Omicron as a “variant of concern.”
COVID-19 cases in South Africa spiked sharply due to the Omicron variant. In mid-November, cases were 300, but by the end of the month, they were 3,000. A COVID-19 tracker from the New York Times reports it’s also been detected in 185 countries.
From the early reports from South Africa, it appeared most cases were mild-and that this variant had different symptoms. In South Africa, patients-many of whom were young-had severe fatigue, but not loss of taste or smell, explains Yale Medicine pulmonologist Lauren Ferrante, MD.
The Omicron variant surged faster than any previous variant in many areas as people around the world ushered in a new year. In the U.S., the new variant led to an increase in caseloads that exceeded the record for new cases per day by the end of 2021. Nevertheless, the number of hospitalizations and deaths was still far lower than when the virus peaked previously.
Related News: 3rd Round Of Free COVID Tests Kits: Here’s How To Order The At-Home Tests
Is Omicron more deadly—or more transmissible—than previous variants?
According to Dr. Murray, scientists were concerned from the start with two critical questions in relation to Omicron. In the first case, it was compared to Delta, earlier variants, such as Alpha and Beta, and the original virus for how transmissible it is.
CDC data indicates that the Omicron variant can spread more quickly than the original SARS-CoV-2 virus and Delta variant, and BA.2 can spread quicker than BA.1.
Grubaugh says if mild infections continue to turn out to be the norm, the rapid transmission would be less of a threat. The second question is whether Omicron—and BA.2—is more likely to cause severe disease than Delta. According to a CDC report published in January, despite the fact that micron has caused a record number of cases and hospitalizations, factors such as lengths of hospital stays, ICU admissions, and deaths are “lower than during previous pandemic peaks.”
According to the CDC, vaccinations, prior infections, age, and other health conditions can influence the severity of symptoms.
How well do current vaccines and treatments protect against severe Omicron disease?
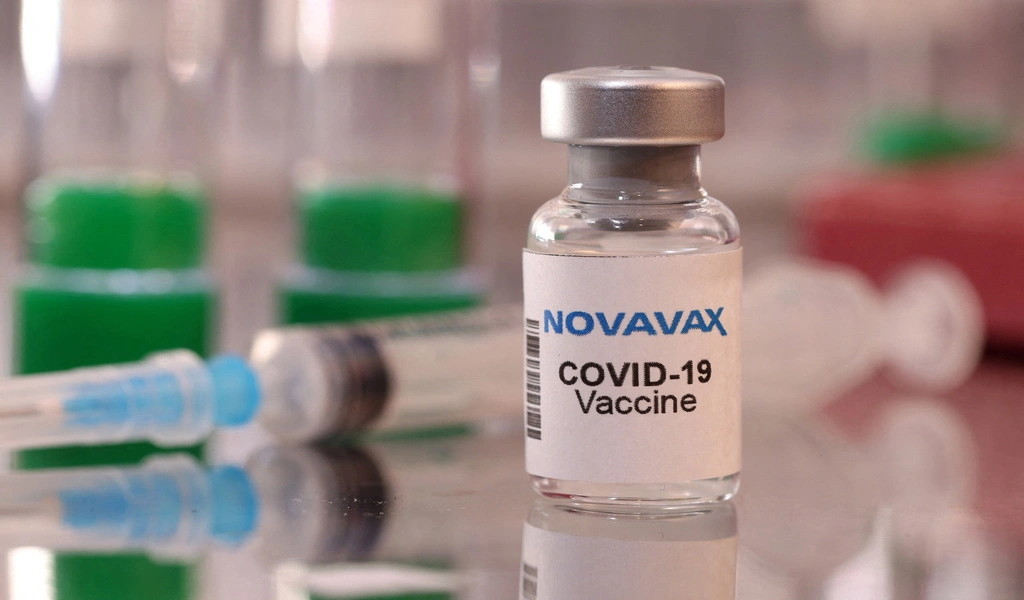
The third question, which is likely to be the most important, is whether or not the existing vaccines will be effective against the new variation, says Dr. Murray. According to research, people who are fully vaccinated and have received booster vaccinations have a strong protection against hospitalization from BA.1 and BA.2.
A key distinguishing factor of Omicron was being discussed shortly after its appearance. There are a lot more mutations in this Coronavirus variant than those in Delta and other coronavirus variants; it contains about 50 mutations, including 26 that are unique to the variant, and more than 30 mutations in the spike protein, the viral protein the immune system is trained to recognize and attack through vaccination. The increased transmissibility of Omicron could be attributed to its ability to evade some immune responses, particularly in people who are previously exposed but not vaccinated. Researchers were also curious if these mutations indicated a possible reduction in the effectiveness of COVID-19 vaccines and certain monoclonal antibodies.
“We don’t really know how these mutations are interacting. It’s not all additive,” Grubaugh had said.
The CDC, however, reported that a third dose, or booster, greatly reduced the need to visit an urgent care facility or hospital due to COVID-19 in January. Earlier this year, the U.S. approved a second booster shot for people older than 50 and those with certain immune deficiencies after early evidence indicated the first booster shot might not prevent the disease.
The FDA has authorized a wide range of monoclonal antibody treatments for both BA.1 and BA.2. As with Evusheld, which is designed to protect people who do not have been infected by BA.1, Paxlovid, molnupiravir, and remdesivir have proven effective against severe BA.1 and BA.2 disease.
Omicron and what you can do to protect yourself
Grubaugh says people need to understand that variants like Omicron and BA.2 are a natural part of the evolution of the virus. “It’s not surprising there’s a new variant,” he says. “There was never going to be a final variant of Delta, and there will never be a final variant of Omicron. Every time there is an outbreak of COVID-19 somewhere in the world, something new will emerge.”
To prevent new variants, Grubaugh and Dr. Murray recommend getting fully vaccinated and getting a booster shot, since more people getting fully vaccinated lessens the likelihood of the virus spreading. In recent years, booster recommendations have changed, and updated information can be found on the CDC website.
Meanwhile, Omicron and BA.2 are stillthreat to U.S. health, and experts recommend that we follow the CDC’s infection prevention guidelines..

Covid-19
WHO Reveals FLiRT Variants as Predominant SARS-CoV-2 Strains in 2024

(CTN News) – The World Health Organization (WHO) has reported that the “FLiRT” versions of the fatal SARS-CoV-2 virus, which causes COVID-19 illnesses, are the most common virus strains this year worldwide.
According to Gulf News, the moniker “FLiRT” refers to the shared mutations on the virus’s spike protein among the variations.
According to the US Centers for Disease Control and Prevention, KP.2, one of the FLiRT variants, has become the most regularly circulating variant in the United States in the last month.
Johns Hopkins University says that the FLiRT variations, which include KP.2’s “parental” lineage JN.1, have three important changes on their spike protein that may help them avoid being caught by antibodies.
Are the FLiRT variations more contagious?
Dr. Aaron Glatt, a representative for the Infectious Diseases Society of America, stated that based on the data he collects and experiences with his own patients, he has seen no evidence of an increase in disease or hospitalizations.
“There have been some significant changes in the variants, but I think in recent times it’s not been as important, probably because of the immunity many, many people already have” due to vaccinations and previous illnesses.
According to CDC data, COVID-19-related hospitalizations have been declining in recent weeks.
Furthermore, the number of patients in emergency rooms who tested positive for COVID-19 has been rather stable over the last month.
Continue to evolve before winter, when infections and hospitalizations often peak, and whether the FLiRT strains will be included in a fall COVID-19 vaccine.
Dr. Roberts answers three questions about the FLiRT variations.
1. Where did the FLiRT strains originate?
Nobody knows where the FLiRT variations first appeared. The CDC initially discovered them in wastewater in the United States, where it screens sewage for signs of SARS-CoV-2 circulating in a community, even if patients do not have symptoms. (The data can be utilized to provide an early warning if infection levels in a community are increasing or decreasing.). FLiRT strains have since been discovered in several other nations, including Canada and the United Kingdom.
To better appreciate how the FLiRT strains developed, consider how the SARS-CoV-2 virus has evolved, with new varieties developing when mutations occur in its genetic coding. Omicron was a SARS-CoV-2 variant that became prevalent in the United States in 2021 and began to produce its subvariants. One of these was JN.1, which was discovered in September 2023 and spread across the country during the winter months, increasing COVID-19 hospitalizations. JN.1 has offspring, including the FLiRT subvariants, which are spinoffs of JN.1.11.1.
2. What do we know—and don’t know—about the FLiRT variants?
We know that the FLiRT variations had two changes in their spike proteins (the spike-shaped protrusions on the virus’s surface) that were not present in JN.1 (the previously prevalent strain in the United States). Some specialists believe that these alterations may allow the virus to avoid people’s protection, whether from the vaccination or a previous bout with COVID.
However, Dr. Roberts believes that the FLiRT variations’ genetic similarity to JN.1 should be reassuring. “While JN.1 occurred during the winter months, when people gather indoors and the virus is more likely to spread, its symptoms were milder than those caused by variants in the early years of the pandemic,” according to him.
There is no word yet on whether a COVID sickness will be more severe with the FLiRT variations or how symptoms may vary. Because everyone is different, a person’s symptoms and severity of COVID disease are largely determined by their immunity and overall health rather than the variant with which they are infected, according to the CDC.
3. How can people defend themselves from FLiRT strains?
Dr. Roberts emphasizes the importance of vaccination as a critical tactic against COVID-19. He recommends that all eligible individuals stay up to date on their immunizations. While immunization does not guarantee immunity, it does dramatically reduce a person’s risk of severe disease, hospitalization, and death from COVID-19.
“We know that the updated monovalent vaccine, which was designed for the XBB.1.5 variant, worked against JN.1, and I strongly suspect it will have some degree of activity against the FLiRT mutations as well,” adds Dr. Roberts.
“I would especially recommend anyone who qualifies for the vaccine because of advanced age get it if they haven’t already,” says Dr. Roberts. “The reason is that the biggest risk factor for a bad outcome from COVID is advanced age.” In the fall of 2023, eligible individuals over 65 can receive the first shot of the revised vaccine and then another shot four months later.
He also believes COVID testing will be able to detect FLiRT strains, and antiviral medications will continue to be effective against them. Paxlovid, the primary treatment for most COVID patients, targets a “nonspiked part of the virus,” he explains. “It’s relatively variant-proof, so it should act against many future COVID iterations.”
Additional preventive measures can assist. To prevent COVID-19, avoiding direct contact with sick people, wearing a mask, washing your hands thoroughly, enhancing ventilation, and monitoring transmission levels in your area is important. Additional options are available on the CDC website.
Covid-19
New Omicron Subvariants, KP.2 and KP.3, Dominate in Canada: What You Need to Know

(CTN News) – More than four years after COVID-19 effectively shut down the world, two new versions of the unique coronavirus have emerged as the dominant strain in Canada.
These new subvariants, KP.2 and KP.3, are classified as Omicron mutations originating from the COVID-19 virus. As of May 19, 49.2% of COVID-19 cases in Canada involved one of these strains, indicating their rapid expansion.
But how much do these subvariants affect the human body? Dr. Isaac Bogoch, an infectious diseases specialist at Toronto General Hospital, believes that while it is too early to say, the most likely outcome is no.
“It’s going to cause predictable symptoms, just like the other sublineages of Omicron,” Bogoch told CTVNews.ca. “Some people will have more serious infection, some will have a milder infection, and some will have no symptoms at all.”
Bogoch, an associate professor at the University of Toronto’s Faculty of Medicine, says the virus’s impact will vary depending on each individual, with factors such as age, health, and underlying medical disorders all playing a role.

Public Health Outlook in Canada
He also claims that the current set of vaccines continues “to do a remarkable job in reducing the risk of serious infection.” Thus, even though the most recent boosters do not account for these new varieties, they still protect the most vulnerable individuals.
However, in the first few months of the subvariant’s existence, there has been no indication that Canadians or public health experts should be concerned.
“The first Omicron wave was terrible, back in late 2021 and early 2022,” he stated. “However, subsequent Omicron waves have had fewer and fewer effects on our healthcare system and society.”
“Of course, this is not to diminish the importance of COVID. “It’s terrible, and certain populations are particularly vulnerable,” he added. “(Both federal and provincial) Public health can do a lot of good by having clear, open, transparent conversations with the general public, just discussing what the current state of COVID-19 is.”

WASHINGTON, DC – DECEMBER 03: People line up outside of a free COVID-19 vaccination site that opened today in the Hubbard Place apartment building on December 3, 2021 in Washington, DC. The DC Department of Health is stepping up vaccination and booster shots as more cases of the Omicron variant are being discovered in the United States. (Photo by Samuel Corum/Getty Images)
Cases have been quite low in the spring and summer, as in the previous few COVID-19 and flu seasons before 2020, before increasing in the autumn and winter.
Bogoch expects the National Advisory Committee on Immunization, Canada’s primary authority on vaccine use, to issue guidelines in the autumn. New COVID-19 injections will be available around the same time as influenza vaccines.
While Canadians have begun to adjust to life after years of pandemic restrictions, cautious optimism is present in the post-COVID world.
Covid-19
Researchers Found Two Extremely Rare Side Effects of the COVID-19 Vaccine

(CTN News) – As millions of people receive their doses of the Covid-19 vaccine, the world is in a race against time to combat the disease. Vaccines have emerged as an integral part of the fight against this pandemic, so ensuring the safety of these vaccines has become increasingly important. As a result of recent studies, it is now known that there are two rare side effects associated with the COVID-19 vaccines, which adds another layer of complexity to the vaccination campaign.
Side effects of the Covid-19 vaccine
Vaccination safety is a broad topic that must be understood before we look at these rare side effects in detail. Common side effects, such as sore arms, fatigue, and mild fever, are well-documented and usually short-lived. Despite the sheer scale of the vaccination campaigns for COVID-19, continuous monitoring is required to identify any unexpected adverse events that may occur.
The Study
The purpose of this study was to analyze data from vaccinated individuals and identify any patterns that might be unusual. The study’s methodology and the diverse pool of participants provided an opportunity to understand potential risks related to vaccines.
Rare Side Effect #1: Allergic Reactions
There have been uncommon allergic reactions following vaccination as one of the rare side effects identified. Even though allergic reactions can vary in severity, the study found instances of uncommon allergic reactions following vaccination. To ensure the safety of vaccine recipients, it is crucial to understand the types and frequency of these reactions.
Rare Side Effect #2: Myocarditis
It is also important to recognize and address the possibility of myocarditis, another rare side effect highlighted by the study, as an inflammation of the heart muscle. Although this is a rare consequence of the treatment, the study emphasizes the importance of recognizing it and addressing it if it occurs.
Impact on Different Age Groups
According to the study, age appears to significantly influence the prevalence of these rare side effects. Also, the study indicates differences in side effects between different age groups, which leads to tailored recommendations for vaccine recipients of varying ages.
Recognizing Symptoms
If you recognize symptoms, you can treat these rare side effects promptly. From allergic reactions to signs of myocarditis, being aware of the warning signs makes it easier for you to seek medical attention right away.
Treatment and Prevention
Although medical interventions for these rare side effects exist, preventive measures can also be taken to protect those at higher risk from experiencing these side effects. Healthcare providers and the general public must be aware of these available choices.
Importance of Reporting Side Effects
Encouraging the public to report any adverse reactions to vaccines is important for ongoing COVID-19vaccine safety monitoring. This collaborative effort between the public and healthcare professionals facilitates a comprehensive understanding of the side effects of vaccines.
Public Awareness Campaigns
The importance of public awareness campaigns plays a vital role in addressing public concerns and misunderstandings. Educating the public about the potential side effects of vaccination and their context and rarity is crucial for maintaining trust in vaccines.
Regulatory Responses
As a result of these findings, health authorities are actively responding to them, adjusting vaccination guidelines and communicating transparently with the public regarding the measures taken to ensure public safety.
Balancing Risks and Benefits
COVID-19Vaccine safety remains a cornerstone of the ongoing assessment of the overall safety of vaccines in the prevention of severe illness and deadly diseases, as it is crucial to balance the risks against the benefits of vaccination in order to make informed decisions.
Future Research Directions
A continued focus is being put on the evaluation of vaccination safety, with a focus on refining vaccination strategies and addressing emerging concerns. The commitment to continual improvement ensures that vaccination programs remain as safe and effective as possible.
Conclusion
As a result, it is imperative to maintain public trust in vaccination efforts if we are to understand and address rare side effects. To avoid the spread of COVID-19 and mitigate its impact, widespread vaccination has proven to be extremely beneficial, and ongoing research and monitoring has enhanced our ability to navigate the complexities associated with COVID-19 vaccine safety.
-

 News3 years ago
News3 years agoLet’s Know About Ultra High Net Worth Individual
-
Entertainment2 years ago
Mabelle Prior: The Voice of Hope, Resilience, and Diversity Inspiring Generations
-

 Health3 years ago
Health3 years agoHow Much Ivermectin Should You Take?
-

 Tech2 years ago
Tech2 years agoTop Forex Brokers of 2023: Reviews and Analysis for Successful Trading
-
 Lifestyles3 years ago
Lifestyles3 years agoAries Soulmate Signs
-

 Movies2 years ago
Movies2 years agoWhat Should I Do If Disney Plus Keeps Logging Me Out of TV?
-

 Health3 years ago
Health3 years agoCan I Buy Ivermectin Without A Prescription in the USA?
-

 Learning3 years ago
Learning3 years agoVirtual Numbers: What Are They For?